Thalassemia is a rare blood disorder characterized by lower-than-normal levels of hemoglobin in the body. Lack of hemoglobin results in lower capacity of carrying oxygen through the red blood cells, leading to anemia. Thalassemia is quite a rare condition; in India, less than a million people are diagnosed with thalassemia every year. A genetic disorder, thalassemia is not completely curable, but effective protocols for management are widely used.
Symptoms & Complications
Thalassemia symptoms can include, but are not limited to:
• Tiredness
• Pale skin
• Lack of physical strength
• Deformities in facial bones
• Stunted growth
• Dark coloured urine
• Swelling of the abdomen
• Pale gums
Thalassemia symptoms can vary widely, depending on whether you have major or mild forms of the disorder. In many mild cases, symptoms will not show u at all. In some people, symptoms of thalassemia will show up right at birth; in some they develop over time. If you are carrying only one thalassemia gene, you will display no visible symptoms.
Patients with thalassemia present with various complications.
• Iron build-up: A build up of iron in the blood is common in thalassemia patients, especially those that require regular blood transfusions. This can be damaging to vital organs.
• Enlarged spleen: Destruction of red blood cells puts extra pressure on the spleen to filter unwanted material
• Bone deformities: Caused by expansion of the bone marrow
• Cardiac problems: Severe thalassemia might lead to arrythmia and congestive heart failure.
Thalassemia Diagnosis
Thalassemia is diagnosed with blood tests. In most cases, children with thalassemia will display symptoms within two years of age. In suspected cases, blood tests are performed to confirm the diagnosis. Pre-natal tests are also available to determine the presence and severity of the disorder.
Thalassemia Treatment
Thalassemia can neither be prevented nor be completely cured, but a host of management options are available.
- Blood transfusions : Cases with severe thalassemia are often treated with frequent blood transfusions. However, this runs the risk of an iron build-up in the blood that causes damage to vital organs.
- Chelation : It is a corrective therapy that removes excess iron form the blood.
- Bone marrow transplant : Also called stem cell transplant, this is the closest to a cure to thalassemia. Administered in cases of severe thalassemia, bone marrow transplants can bypass the need for lifelong blood transfusions and excessive medications.
What Is Bone Marrow Transplant?
Healthy blood forming bone marrow is taken from the donor and infused into the body of the patient, replacing the disease bone marrow. Donors are matched based on the blood type, and can be anonymous, family, or an acquaintance.
Healthy stem cells are collected from either the donor’s blood, the bone marrow from the donor’s hipbone, or from an umbilical cord.
During the transplant, the patient will undergo various preparatory procedures. These may include:
• High-dose chemotherapy to kill off the diseased cells
• Infusion of healthy stem cells into the bloodstream
• Various tests and medications designed to monitor the success of the stem cell transplant and manage complications, if any
• Blood transfusions (in some cases) for a few weeks while the new cells settle in before positive results start showing
Around 10 to 15 thousand children are born with thalassemia each year. While this disease is not preventable, adequate care, a healthy lifestyle, early diagnosis, and ultimately a bone marrow transplant can allow these children the best chance at living a fulfilling life.
One of the most widely used treatments for cancer today is radiotherapy or radiation therapy. According to statistics, currently, about 60% of patients diagnosed with cancer in India will require radiation as part of their treatment. However, there are still many questions in the minds of patients about this therapy. Such as, at what stage of cancer is radiotherapy effective? Is this procedure painful? How successful is radiotherapy in the fight against cancer? The Head of the Department of Radiation Oncology at Apollo Multispeciality Hospitals, Dr Tanweer Shahid gives us the answers.
What is Radiation therapy or radiotherapy? Dr Shahid says, “Radiation is high energy X-rays which are directly focused on the patient’s tumour cells. It attacks the cells directly and causes damage to the cancer cells inside the tumour.” Radiation works by breaking down the water inside the affected cells, turning it into compounds that kill the tumour cells from the inside out.
According to Dr Shahid, there is consensus among the medical community regarding radiation therapy being an ideal treatment for cancer. Likewise, it is often used in conjunction with other therapies such as chemotherapy or surgery. However, a valid question that arises is, does radiotherapy also damage the good cells of the body like chemotherapy? The answer is that in many cases, radiotherapy does damage healthy cells, particularly in areas adjacent to the tumour cells, but this is not permanent and the cells do renew themselves. Also, as the treatment is highly targeted, doctors apply it only to the tumour and there are no other generalised side effects, like hair loss, elsewhere in the body.
What are the stages of cancer where radiotherapy can be used? There are a number of different cases where the oncologist might use radiotherapy. Firstly, it is used as the main treatment for cancer. It can also be used in conjunction with surgery: pre-surgery to reduce the size of a tumour or post-surgery to eradicate any remaining cancer cells. Finally, it also finds application in reducing the symptoms of end-stage cancer. Speaking of the duration of the treatment, Dr Shahid tells us that that is dependent on the stage of the cancer.
Finally, let’s take a look at the side effects of this therapy. In Dr Shahid’s words, although there are certain side effects, these are neither major nor permanent. For example, there are no generalised side effects, and no pain or discomfort in the affected area. Patients do experience localised skin pigmentation and hair loss in the area where the radiation is being applied. However, these effects vanish soon after the therapy is complete and the hair eventually grows back.
Physicians across the globe believe that a patient’s state of mind and mental well-being plays a key role in his or her fight against this disease. However, the stress and anxiety arising from constantly worrying about the quality of treatment one is getting can be detrimental to the patient. At Apollo Multispeciality Hospital, Kolkata, patients are given the best facilities, treatment and care, so that they can leave the worries and stress to the doctors and completely focus on getting better and beating cancer.
This report is published in a joint venture with Apollo Hospital Kolkata.
A myocardial infarction, commonly known as a heart attack, is a serious medical emergency. It is an extremely common and rising cause of hospitalization across the globe. anyone suspecting a heart attack should immediately visit the nearest hospital in order to receive medical assistance. A heart attack is a life-threatening condition, and time is of essence in its treatment.
What Causes Heart Attacks?
A heart attack is caused by an obstruction to the arteries, usually by a blood clot, causing it to get blocked and stop working. The longer it takes for the artery to open up and get working again, the less the chances of the patient returning to a normal life. As blood flow stops, the heart muscles begin to die. Irreversible damage will lead to a cardiac arrest, causing death.
Signs Of A Heart Attack
It is important to keep in mind that a heart attack can mimic the symptoms of other, far less severe conditions. It is therefore imperative to take these symptoms seriously, especially if there is history of heart disease. It should be noted, however, that heart attacks can happen without any pre-existing heart conditions.
Chest pain: The commonest symptom of a heart attack is chest pain. Someone experiencing a heart attack may feel a tightness across the chest. The pan might feel severe or very mild depending on the severity of the attack.
Shortness of breath: Patients might experience difficulty breathing or attempt to take in a lot of air by opening their mouth. This might be accompanied by sudden weakness and fatigue.
Radiating pain: The chest pain may appear to radiate to the arms and legs. This is most commonly seen spreading to the left arm, but might also involve the right. Pain in the back, jaw, and neck is also possible.
Dizziness: Patients might also feel lightheaded, accompanied by bouts of vomiting.
Sweating: Sudden, excessive sweating is a symptom of a heart attack.
What Causes Heart Attacks?
Coronary Heart Disease is the leading cause of heart attacks. The coronary arteries get clogged with cholesterol deposits. Eventually, a plaque bursts, causing a blood clot that triggers a heart attack. CHD is caused by smoking, high cholesterol, obesity, a high-fat diet, lack of exercise, diabetes, and hypertension.
Hypoxia occurs when the heart receives unoxygenated blood due to an impairment in lung function or carbon monoxide poisoning. Lack of oxygen will damage the heart muscles, leading to a heart attack.
Drug misuse can also narrow down the coronary arteries, resulting in decreased blood flow and eventual heart attacks.
How Are Heart Attacks Treated?
As stated before, time is of the essence when treating heart attacks. The sooner the patient receives emergency medical attention, the better the prognosis. Of course, this also depends on the severity and type of attack.
Medical assistance for a heart attack will vary widely.
Medications
A range of medicines can be administered to the patient, mainly aimed at reducing pressure on the heart. A combination of blood thinners, beta blockers, and pain relievers along with medicines to bring down the cholesterol and blood pressure will be administered to keep the heart muscles from working overtime.
Surgery
Patients might also be suggested surgical procedures to help contain and/or reverse the damage.
Angioplasty and stenting involve inserting a stent into the blocked artery to remove the clot and allow blood to flow. Usually, the stent is coated with medicine to prevent further clots from forming.
Coronary bypass surgery involves guiding the blood flow to bypass the blocked parts of the artery. This might be an emergency surgery, or the patient might be given a few days to stabilize before undergoing the procedure.
The importance of swift medical intervention cannot be stressed enough in case of a heart attack. It is essential, therefore, to be educated on the symptoms of a heart attack to be able to seek out assistance at the earliest. Most importantly, a healthy lifestyle is paramount in keeping potentially debilitating heart diseases at bay.
Balloon Dilatation is a safe and minimally invasive procedure to treat tracheal stenosis. The post-Covid era has seen a significant increase in the number of patients developing tracheal stenosis due to spending a prolonged period of time on ventilator support.
What Is Tracheal Stenosis ?
The Trachea or The Windpipe is the airway bridging the lugs and the voice box. Narrowing or constriction of the windpipe is called tracheal stenosis. It results in restricted airflow and hinders the ability to breathe normally.
Symptoms & Diagnosis
Tracheal stenosis can be congenital or acquired. Stenosis might develop following an injury or an illness. In most cases, tracheal stenosis is seen in patients that have been intubated or ventilated for a prolonged period of time.
Diagnosis of tracheal stenosis can be a little tricky since the symptoms are similar to those of other conditions. In general, tracheal stenosis might present the following:
• A general feeling of being unwell
• Shortness of breath
• A wheezing of shrill sound coming from the lungs when breathing
• Recurring URIs or pneumonia
• Apnea
• Bluish tint to the skin and mucous membranes
Treatments For Stenosis
Balloon Dilatation is a common procedure performed top ease the symptoms of tracheal stenosis. The purpose is to increase the width of the trachea so that the patient is able to breathe more easily. The procedure is performed under anesthesia, through the mouth. An incision is made in the narrowed portion of the airway, and a high-pressure balloon dilator is applied to widen the trachea. Medications are administered to prevent formation of scars that might further narrow the airway.
Apart from balloon dilatation, stenting and surgical reconstruction of the airway are also considered, depending on the severity of the stenosis.
Rheumatoid arthritis is an autoimmune disorder that results in chronic inflammation- not just of the joints but also several other parts of the body. It is a deforming symmetrical arthritis that mostly affects the small joints of the hands and feet and larger joints like the wrists, elbows, hips, and shoulders. It can progressively affect the eyes, lungs, marrow, spleen, and blood vessels among other parts. Although there is no cure yet, standard treatments have currently been supplemented by very effective biologic and small molecules treatments.
What are the symptoms?
Some of the early symptoms of rheumatoid arthritis are swollen joints that are painful to the touch. Patients may feel the pain and discomfort worsening after periods of inactivity, and the symptoms to improve with exercise. In the early stages, the smaller joints will be affected, particularly the fingers and the toes. As the disease progresses, similar pain and discomfort will start to affect additional areas such as the ankles, wrists, elbows, knees, hips, and shoulders.
Patients may also experience problems in areas other than the joints, such as skin, eyes, salivary glands, heart and kidneys. Rheumatoid arthritis also affects the nerves, bone marrow and blood vessels.
It is important to note that rheumatoid arthritis symptoms can come and go. Only a proper treatment plan can most effectively manage this condition and suppress symptoms for prolonged periods.
How is it diagnosed?
Rheumatoid arthritis will be diagnosed by your physician after conducting a series of clinical tests and physical examinations. As the early symptoms of this conditions mimic that of several other diseases, doctors need to perform a number of tests to eliminate other possibilities. A physical exam will include checking your joints for inflammation, and also a test of muscle strength and reflexes. Blood and imaging tests will also be conducted to look for inflammation and determine the degree of damage to the bones.
What is the treatment?
An early diagnosis is crucial to the treatment and eventual remission of symptoms in rheumatoid arthritis. A proper treatment plan specifically suited to your requirements will take into account the severity and duration of the disease.
A combination of medication and therapy is recommended in the treatment of rheumatoid arthritis. Non-steroidal ani-inflammatory drugs are prescribed to reduce pain and inflammation. Corticosteroids help in slowing down joint damage. Disease-modifying anti-rheumatic drugs or DMARDs are extremely beneficial since they not only alleviate symptoms, but also significantly slow down joint damage and [prevent irreversible damage.
In more severe cases of rheumatoid arthritis, patients are administered biologic response modifiers or biologic agents. These drugs help in locking he immune system chemical reactions, thus preventing inflammation and tissue damage.
Patients may also require physical or occupational therapy to manage the symptoms, along with medications. Assisted devices might come into play as well. In severe cases, surgery might also be recommended to repair or replace damaged joints.
Rheumatoid arthritis is a chronic condition. Today, medical science has made progression in leaps and bounds that have very successfully managed the condition to the point of remission. However, I is of utmost importance that the patient seek out the expertise of a rheumatologist at the earliest in order to receive the most effective treatment that will ensure maximum return to normalcy.
Emergency Medicine: Life-Saving Speciality
Emergency medicine is an emerging faculty in India, being recognized as a specialty only in 2009. As the name suggests, emergency medicine professionals are specially trained in caring for unscheduled patients of undifferentiated age and medical histories. Emergency doctors are involved in cases requiring immediate and urgent medical attention, and are responsible for the resuscitation and stabilization of critical patients.
Emergency medicine doctors are first-line providers, and the lineup consists of internists, pediatricians, surgeons, general practitioners, cardiologists, and neurosurgeons, depending on the emergency. A team of professionals in the emergency department needs to be equipped with the ability to treat patients with minor injuries or illnesses and release them post-treatment, and also cater to critically ill patients requiring intensive care and/or resuscitation.
On any given day, an emergency medicine doctor will cater to patients from all walks of life, irrespective of age, sex, and medical history. In some cases, such as trauma from an accident/attack or a stroke, the doctor will begin treatment immediately. In other cases, such as a particularly critical complication arising from an existing condition, the doctor will attempt to stabilize the patient and commence with treatment post assessment of the patient’s medical history.
A well-equipped emergency medicine facility is crucial at every hospital. On a day-to-day basis, the emergency departments are faced with a large number of patients requiring immediate medical assistance. This line of medicine is particularly essential in times of crisis, as evidenced by the Covid-19 pandemic. Similar situations arise in cases of natural and man-made disasters, terrorist attacks, and accidents.
Apart from an experienced team of doctors and nurses, emergency departments are also aided by state-of-the-art medical equipment designed to stabilize and treat patients as necessary.
Fetal medicine is a speciality that deals with the care of babies in utero. In recent times, great advancements in the field of fetal medicine have increased manifold the chances of a successful pregnancy by attending to issues with the baby in utero.
when to see a fetal medicine specialist?
Fetal medicine specialists deal with:
- High-risk pregnancies
- Pregnant women with chronic conditions such as diabetes, hypertension, heart/kidney disease, blood disorders
- Possibilities of pregnancy-related complications such as pre-eclampsia, preterm labour, or multiple births
- At-risk fetuses with congenital or chromosomal abnormalities, genetic diseases, or stunted growth
- Unforeseen pregnancy-related complications that might arise while the mother is expecting, such as gestational diabetes
- Birth defects such as spina bifida, chest and heart malformations, and kidney issues, among others
- Diagnosis or history of cancer in the mother
- Possibility of trauma to the mother and child due to an accident/injury
Pre-Existing Conditions
Fetal treatment options consist of careful administration of medications and prescribing a strict lifestyle for successful completion of pregnancy.
Cancer
In case of the mother has or is undergoing cancer treatment, pregnancy is likely to cause more stress to a system already stressed out by cancer treatment. In such cases, fetal medicine specialists will consult with the oncologist to map out a treatment plan that minimizes risk to the baby while benefiting the mother.
Trauma
In cases of trauma, immediate surgical intervention might be required- depending on the severity of the injury- to save both the mother and the child.
Birth Defects
Advanced fetal treatment options are available to repair certain defects before birth. For instance, spina bifida can be corrected in utero by opening up the uterus, while other procedures are performed endoscopically by inserting tiny cameras through minimal incisions.
Incomplete Pregnancy
In case the mother presents with a history of a miscarriage or preterm labour, fetal medicine specialists will work towards diagnosing a possible cause for the unsuccessful pregnancy in order to prevent it from recurring. Management can range from lifestyle change and medications to surgical intervention.
The advancement in fetal-maternal medicine has brought down the mortality rate among newborns and mothers alike by a significant percentage.
A kidney transplant is a surgical procedure that replaces a non-functional kidney in a body with a healthy kidney from a donor- deceased or living. It’s a life-saving procedure usually undertaken in those with end-stage kidney disease. Traditionally, kidney transplantation has been performed via open surgery, involving making large incisions on the body. In recent times, Robot-Assisted Kidney Transplant has replaced open surgery as the choice of procedure for kidney transplants.
Why Is Kidney Transplant Performed?
End-stage kidney disease culminates in kidney failure when 90% or more of the kidney ceases to function properly. Responsible for filtering waste materials from the body, a non-functioning kidney will result in the build-up of toxins in the body, leading to an often very painful death. The only other treatment for the management of renal failure is a lifetime of dialysis or the removal of waste material from the body via a machine.
- Kidney transplantation is the most sure-shot way of ensuring a longer lifespan with a significantly improved quality of life.
- The risk of death is much lower as compared with dialysis.
- A transplanted kidney allows the person to live a relatively normal life with significantly fewer dietary restrictions, although a much healthier lifestyle always ensures better chances of success with the transplant.
- The one-time surgical cost is much lower as compared to a lifetime of dialysis, medications, and frequent doctor visits.
Who Is Eligible?
Kidney transplantation is performed in persons with acute kidney failure, chronic kidney disease, or end-stage renal disease. Persons prescribed dialysis might also benefit from kidney transplantation before the treatment cycle begins.
Open Surgery Vs. Robot-Assisted Kidney Transplant
In open surgery, a large incision is made on the patient’s body. The diseased kidney is removed and the healthy organ is replaced.
In RAKT, two much smaller incisions are made on the body. The diseased kidney is removed and the healthy kidney replaced through the larger of the incisions, while the instruments are entered into the site of surgery through the other.
Benefits Of Robot Assisted Kidney Transplant
There are significant advantages of RAKT over traditional open surgery.
- The robotic instruments assisting in the surgery are more flexible and manoeuvrable than human hands, resulting in lower chances of accidents in a delicate surgical procedure.
- Since the incisions are much smaller, it takes fewer days for the patient to recover, bringing down the cost of a hospital stay.
- A small wound means less blood loss, less pain and lower chances of infection.
- Smaller wounds mean a better cosmetic outcome.
How To Prepare?
A candidate for kidney transplant is required to undertake a strict lifestyle before they undergo the surgery. It is imperative that they
- Lose excess weight
- Quit smoking and drinking
- Maintain an active lifestyle
- Undertake all necessary tests
- Receive dialysis treatments
How Successful Is RAKT?
Generally speaking, Robot-Assisted Kidney Transplants have a higher rate of success than open surgeries. However, it is important to note that success depends greatly on the overall health and lifestyle of the patient.
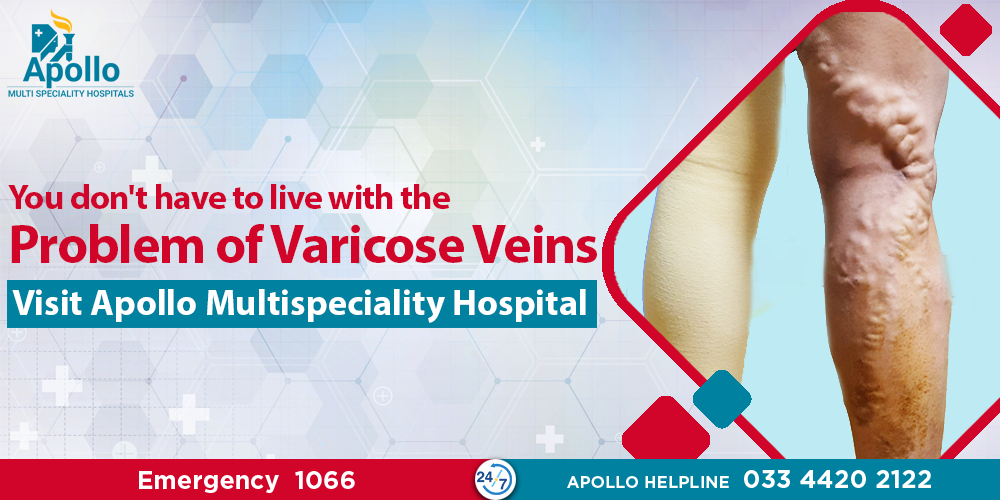
Looking For An Effective Treatment For Varicose Veins? Read On…
It is estimated that about 7% of the normal Indian population suffers from Varicose Veins. You yourself may have observed the condition – knotted, dark and bulging veins in the legs, often concentrated around the calf. If detected in the early stages, one need only follow the doctor’s instructions and make small changes to prevent the condition from progressing. But the questions remain – what are varicose veins, what are the symptoms and how can the condition be treated? We bring you all the answers straight from Dr Manas Saha of Apollo Multispeciality Hospitals, Kolkata.
So, what are Varicose Veins? Dr Saha informs us that it is a condition where the veins in our legs are dilated and appear stained and bulging. The exact cause of the condition is yet unknown. However, it is mostly observed in people who spend considerable amounts of time on their feet for professional or personal reasons, such as chefs, traffic policemen or housewives. It has been postulated that standing for long periods of time puts more pressure on these veins than they are meant for, leading to the condition.
And, how would you know if you have Varicose Veins? The most common sign is dilated bulging veins in the calves or the entire leg. Another common symptom may be continuing pain and swelling of the legs, especially in the evening. However, the symptom that Dr Saha particularly warns us about is a discolouration of the legs, with deeply stained veins, some of which develop ulcers that refuse to heal even with treatment. This is a sign of heavy congestion in the veins, and should never be left untreated.
Speaking of treatment, Dr Saha informs us that is most cases where Varicose Veins are asymptomatic, no treatment is required. However, in cases of asymptomatic patients in showbiz or aviation, or those with severe symptoms, there have been a few different treatment options. These options are surgery and thermo-ablation. Both treatments are painful, done under heavy anaesthesia, bring with them the threat of complications and have a high recurrence rate. In spite of the problems, a lengthy and expensive combination of surgery and ablation has so far been used to treat Varicose Veins.
But here, Dr Saha brings us some good news. With the technique developed and modified in their institute, there is now a third form of treatment which has “no surgery, no stitches, no anaesthesia”, i.e. Venous Occlusion of the Varicose Veins. This procedure is carried out by injecting a special glue in pre-determined doses into the Varicose Veins and while the veins take some time to disappear, the symptoms are gone almost immediately. The procedure is relatively simple, completed in a single session and has a minimal rate of recurrence. Followed by
proper care and wearing of the prescribed stockings, this revolutionary technique offered at Apollo Multispeciality Hospitals, Kolkata could free you from Varicose Veins for life.
This report is published in a joint venture with Apollo Multispeciality Hospital, Kolkata.
Spinal problems can manifest in many forms — ranging from mild issues requiring minimal medical intervention to serious conditions requiring surgery
Common Spinal Disorders
Some of the common spinal disorders are:
- Scoliosis: A common spinal disease in which the spine has a curvature like an S or a C.
- Lumbar spinal stenosis: The spinal canal at the end of the vertebrae narrows, resulting in a pinching of the nerve roots of the spinal cord. This leads to pain in the legs and lower back.
- Spinal Infections: Most commonly spinal bones tuberculosis
which may lead to paralysis
Treatment Plans
Both surgical and non-surgical methods are adopted in the approach to treating spinal diseases. The medical team studies the patient’s symptoms and case history and adopts a treatment plan best suited to the scenario.
Non-Operative Methods
In most cases of spinal diseases, non-operative methods are undertaken. Non-operative procedures include, but are not limited to:
- Targeted injections
- Rehabilitation therapy
- Pain management
- Heat and Cold therapies
- Exercises
Operative Methods
Operative methods are undertaken for deformity correction, relieving pressure from pinched nerves and spinal cord, removing infective material and sometimes for diagnostic biopsies. Spinal surgeries can range from being minimally invasive to very complex procedures involving reconstruction of the spine. Spinal surgeries include, but are not limited to:
- Complex spinal reconstruction
- Disc replacement
- Revision spine surgery
- Complex deformity correction
- Spinal implantation
- Lumbar fusion
- Vertebroplasties
- Balloon Kyphoplasty
Due to the sensitive nature of the spinal cord, surgeries are undertaken with great care, and specialists strive to be as minimally invasive as possible. With the great strides taken by medical science, robotic aids have greatly improved the success rates of spinal surgeries. Coupled with medical advancements and a comprehensive follow-up plan for rehabilitation, spinal surgeries today come with the promise of a return to a healthy and normal life. Greatly improved the success rates of spinal surgeries. Coupled with medical advancements and a comprehensive follow-up plan for rehabilitation, spinal surgeries today come with the promise of a return to a healthy and normal life.
Minimally Invasive Cardiac Surgery Or Smart Cardiac Surgery has evolved in the last decade. The Cardiac Department at Apollo Multispecialty Hospitals has honed these surgical techniques to the maximum possible benefit of the patients.
Why MICS?
Coronary vascular disease or CABG surgery is a major procedure, involving bone-cutting. Open surgery results in a long hospital stay, significant restrictions in lifestyle and movement following release, and overall a much longer recovery time. Minimally Invasive Cardiac Surgery, on the other hand, optimally reduces all the aforementioned timeframes, thus allowing a much faster return to normal life.
Which Operations Are Performed?
Nearly all the major cardiac surgeries can be performed through this route. Principally, the following surgeries are performed:
- Coronary artery bypass surgery
- Valvular heart diseases
- Operations on the holes of the heart
- Removal of cardiac tumours
- Pacemaker implantations
The Procedure
This surgery involves very small cuts in the sides of the chest between the ribs. Several types of MICS are performed, depending on the patient’s requirement.
- Partial Sternotomy: The surgeon reaches the heart through a 3-4 inch incision made through the sternum so the breastbone can be separated.
- Mini-thoracotomy: Instead of the breastbone, the surgeon cuts through the muscles between the ribs.
- Robotically-assisted heart surgery: Surgical instruments are attached to robotic arms and controlled by the surgeon, which performs the surgery through the incision
Benefits Of MICS
- Lower blood loss: The patient loses much less blood than would occur during a traditional open-heart surgery
- Lower chances of infection: A smaller and less invasive incision results in much lower chances of contracting an infection and further complications
- Minimised trauma and pain: Post-operative discomfort and pain are much less since the breastbone remains unbroken and the incision is much smaller
- Reduced hospital stay: The patient can be discharged within a week from the date of the surgery with instructions for further care and management
- Quicker recovery: MICS ensures minimum trauma to the body, so the patient heals much quicker instead of the months that follow open-heart surgery
- Less noticeable scarring: A smaller incision means a much less noticeable
scar
Nearly all patients are eligible for Minimally Invasive Heart Surgery. Your doctors will determine whether you are a candidate for MICS taking into account your age, medical history, and prognosis.
In India, about 15 lakh patients are diagnosed with prostate cancer every year, out of whom about 85 per cent are diagnosed in stage four. The prostate gland is a small walnut-shaped gland placed just below the urinary bladder in males. It produces and contains a fluid that forms part of the semen, which in turn helps in maintaining sperm health. If prostate cancer is detected in stage one, the recovery rate can be 100 per cent. However, if there is a delay in detection and it is diagnosed in stage four, the chances of cure come down to 28 per cent.
“Prostate cancer must be detected early to ensure a full recovery. About one in six men may have prostate cancer in their lifetime. If there’s a family history of prostate cancer — if one’s father, brother, son or even an uncle had the disease — one in five men could develop prostate cancer in their lifetime,” pointed out Dr Indraneel Banerjee, consultant, uro-oncologist, and robotic surgeon at Apollo Gleneagles Hospitals, Kolkata.
One way of early detection of prostate cancer is through prostate cancer screening, which usually involves a blood test and a physical examination. Screening should be done even when there are no symptoms, as it is possible for prostate cancer to develop even without any urinary dysfunction.
“Asymptomatic men in the age group of 55 to 69 years should get themselves screened for prostate cancer. For those between 40 and 54 years, screening is advised only if they have a family history of prostate cancer or have urinary symptoms. For those above 70 years, screening is generally not recommended. But if a man aged over 70 years is in good health and expects to live for another 10 to 15 years, or is on regular medication, screening can be done,” explained Dr Banerjee.
Among the blood tests conducted for prostate cancer detection is the Prostate Specific Antigen (PSA) test. Dr Banerjee warned patients that even though a PSA reading of less than 4 is often assumed to mean there is no chance of prostate cancer, it is advisable to consult a urologist or an uro-oncologist to interpret the test results and receive confirmation as the test results depend on many factors. In some cases, advanced imaging studies like an MRI scan or a prostate biopsy may be necessary.
Near complete cure (90-100%) is possible only with surgery if the patients are diagnosed with localized low or intermediate-risk group prostate cancer. In high-risk group patients, as part of the of multi-modality treatment, the patients may need radiation therapy after surgery. However, as compared to radiation therapy, most of the patients do not need a hormonal injection after surgery and with the removal of the prostate gland, the urinary symptoms are also relieved. With the advent of Robotic surgery, the patient will have less pain-less blood loss and shorter hospital stay as compared to open surgery.
In case prostate cancer is detected late, radiation, instead of surgery, is the preferred option. “Radiation has the potential to work at all stages of prostate cancer, including the fourth stage when there is limited metastasis. Studies show that side effects are far less in case of radiation. As such, radiation is a painless and non-invasive procedure,” said Dr Sayan Paul, senior consultant and radiation oncologist, Apollo Gleneagles Hospitals, Kolkata.
Besides surgery and radiation, a third alternative is the use of medicine for therapy, as summarized by Dr Indranil Ghosh, consultant, and medical oncologist, Apollo Gleneagles Hospitals, Kolkata: “Hormone therapy is generally what is used to control cancer in most patients; it has very few side-effects. If cancer has reached the last stage and spread considerably, one can go for chemotherapy. Nowadays we also have targeted therapy that is based on the genetic analysis of the tumour and is designed to achieve absolute precision.”
Notwithstanding the various treatment options, a frequently asked question among patients remains, how to stop prostate cancer in the first place?
“There is nothing specific to recommend. Just lead a healthy life, do your share of exercises and eat a balanced diet,” said Dr Banerjee.
দ্রুত শনাক্তকরণই প্রোস্টেট ক্যানসার সম্পূর্ণভাবে নিরাময়ের একমাত্র উপায় ➡
Press Release
Our Clinical Team

Dr. Mahesh Kr. Goenka

Dr. Indrajeet Kumar Tiwary

Dr Nikhil Sonthalia

Dr. Awanish Tewari

Dr Vikash Prakash

Dr. Bhavik B Shah D

Dr. Kinsuk Das

Dr Pankaj Kumar
The Procedure
In the media
- The Echo of India, Pg 8 – Apollo Multispecialty Hospital Kolkata brings power spiral Enteroscopy to investigate and treat gastro-intestinal tract diseases
- Morning India, pg 2 – Apollo Multispecialty Hospital Kolkata brings power spiral Enteroscopy to investigate and treat gastro-intestinal tract diseases
- Ei Samay, pg 6 – New treatment for gastro-intestinal tract diseases
- Arthik Lipi, pg 8 – For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
- Prabhat Khabar, pg 5 – Apollo Multispecialty Hospital Kolkata brings power spiral Enteroscopy to investigate and treat gastro-intestinal tract diseases
- Bharat Mitra, pg 6 – Apollo Multispecialty Hospital Kolkata brings power spiral Enteroscopy to investigate and treat gastro-intestinal tract diseases
- Janpath Samachar, pg 12 – Apollo Multispecialty Hospital Kolkata brings power spiral Enteroscopy to investigate and treat gastro-intestinal tract diseases
- 24×7 Taaza Samachar
– For the first time in Eastern India, Apollo Multispecialty Hospitals
Kolkata brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - New India Broadcast
– For the first time in Eastern India, Apollo Multispecialty Hospitals
Kolkata brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - Shubhabori
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata brings
Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - 24×7 News Bengal
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata
brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - iBG News Bengali
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata
brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - iBG News English
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata
brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - Biswa Bangla News
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata
brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - News A Bangla
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata
brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - Bengal News Grid
– For the first time in Eastern India, Apollo Multispecialty Hospitals Kolkata
brings Power Spiral Enteroscopy to investigate and treat gastrointestinal tract diseases
Read More - Financial Samachar
– Power Spiral Enteroscopy to investigate and treat gastrointestinal tract
diseases
Read More